While many acute care settings use electronic pumps to calculate IV flow rates, there are many scenarios in which nurses need to know how to calculate drip rates manually! For example, when working in rural or low-resource environments, electronic intravenous pumps may not be available. Even when electronic pumps are available, nurses should know how to verify drip rates, especially for high-risk medications. Nurses should verify the drip rate at least once per shift or when a new medication/fluid is started or titrated.1
Electronic pumps deliver fluids and/or medications using positive pressure to deliver a constant amount of solution per hour. If available, the nurse should use electronic IV pumps because they are more accurate than manually adjusting the rate to be delivered by gravity. However, the nurse must also double-check the orders for rate of medication administration when using electronic pumps. This includes checking that the drip rate is in the therapeutic dosage range for that patient.
What is an IV drip rate?
The drip rate describes the number of drops per minute an IV delivers to the patient, whether through a pump or by gravity. However, a drip rate is not a drug dosage, since different IV tubes deliver different volumes of drips that would contain different amounts of medication. Therefore, a prerequisite for calculating the drip rate is knowing which IV tube you are using to deliver the drug or fluid. We will explore this concept in more detail in the next sections.
Simply put, the IV drip rate is the number of drops of fluid administered to the patient per minute. Then, the concentration of the drug in the fluid, the size of the tube and the drip rate influence the dosage of the drug / fluid.
What is gtt?
One place that new nurses often get lost is the idea of gtt. Why is it called gtt? Many scientific names originate from Latin—the abbreviation of gtt came from the Latin name for drop, which is gutta and for plural drops, guttae. Conceptually, gtt and drop mean the same thing, so if nurses are more comfortable writing “drops” anywhere in equations where gtt shows up, that can ease confusion.
Gtt/ml Conversion & Drop Factor
Converting gtt (drops) to ml is important because medication or fluid orders are generally given in ml/hour rather than in gtt.
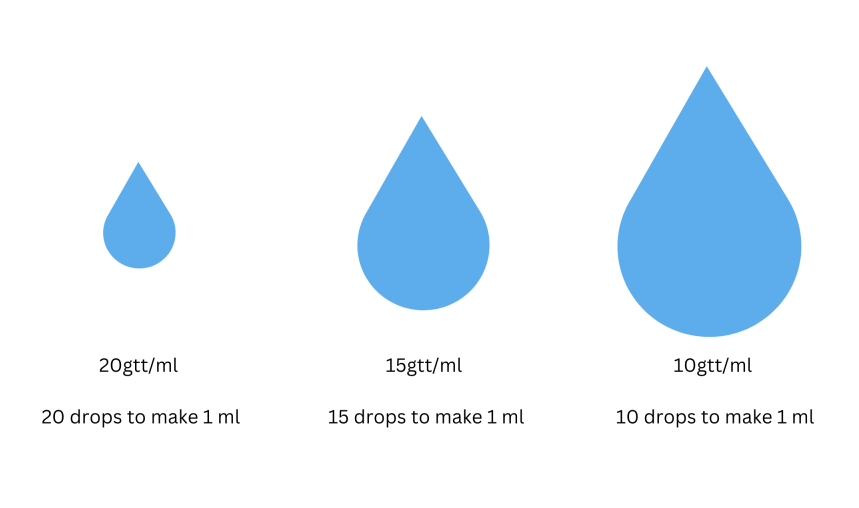
To convert gtt to ml or vice versa, the nurse must know what kind of tubing they are going to use. Some IV solutions require specific tubing (such as blood products), or electronic pumps may have specific tubing that is compatible. Regardless, the nurse should be familiar with the gtt/ml of the tubing they are using. The gtt/ml (drops per ml) is equivalent to the “drop factor” of the tubing. Tubing sets should list their drop factor on the packaging. For example, 10 gtt/ml (drop factor of 10) means it takes ten drops to make one ml of fluid, 15 gtt means it takes 15 drops to make 1 ml of fluid, and so on.
Micro vs Macro tubing
IV tubing is generally classified as macro tubing or micro tubing. Macro tubing is used to deliver larger fluid volumes. Macro tubing should be used when delivering more than 80 ml of fluid per hour.2 Macro tubing is also called standard tubing in practice and usually delivers either 10, 15, or 20 gtt/ml (drops/ml). It is always important that the nurse double checks on the packaging what the drops per ml are for safe drug calculations.
Microtubing is used to deliver very precise or small amounts of fluids. Microtubing is also used for pediatric and neonatal patients. Micro drip tubing is usually set to 60 gtt/ml (60 drops to make 1 ml).
How to Calculate Drip Rate
To manually measure the IV drip rate, the nurse needs to be able to calculate gtt/min, which means the number of drops from the IV tubing measured over 1 minute. For efficiency, drops per minute can be divided by 2 (count drops for 30 seconds) or 4 (count drops for 15 seconds). The nurse would then multiply number of drops by 2 (30 seconds) or 4 (15 seconds to get the drip rate. Gtt/mins and drops per minute both are equivalent to the drip rate.
There are three basic components that you need to calculate the drip rates:
- Total volume to be infused
- Drop factor of the tubing
- Amount of time to be infused over
Conceptually this is the formula for calculating the drops/minute:
Total volume x drop factor ÷ time = flow rate (gtt (drops)/min)
Adding in the correct units of measurement, this is the formula:
Drip rate in drops/minute = (total ml ÷ total minutes) X drop factor in drops/ml
An issue that often comes up is that a fluid or medication order might be written in other units of measurement, such as fluid in liters or time in hours.
Here the steps are completely broken down to initiate a new order:
Example 1
Step 1: Check the order. In this case, the order reads: Bolus 1000 ml normal saline over 6 hours.
Step 2: Assemble supplies. Check what the drop factor is on the standard tubing. In this case, the standard tubing is 10 gtt(drops) /ml.
Step 3: The units on the order don’t match the units on the drop rate formula, so the nurse must convert the units to match.
6 hours x 60 minutes/hour = 360 minutes
1 liter X 1,000 ml/L = 1,000 ml
Step 4: Input order with converted units into the drip rate formula.
(1,000 ml ÷ 360 minutes) x (10 gtt ÷ 1 ml)
= (1,000 ÷ 360 minutes) x 10 gtt
= 2.78 X 10 gtt
= 27.8 drops/minute
= rounded 28 drop/minute
On a practical level, if the fluid or medication is being delivered by gravity. How does the nurse go about changing the drip rate? If the nurse is manually changing the drip rate, they would watch the drops while counting to 15 seconds. Then take the number of drops and multiply by 4 to get the drip rate. The nurse then manually adjusts the IV tubing until the correct number of drops are falling over the 15 seconds.
If delivered by an electronic pump, the nurse would program the pump, then check the drip rate once the pump is running to ensure that the pump is running and programmed correctly.
Example 2
Step 1: Check the order. In this case, the order reads: Heparin 20,000 units in 500 mL D5W is ordered to run at 2,000 units/hour.
Step 2: There is an extra step here because the order is in units rather than ml per hour. To calculate the concentration of heparin in the bag 20,000 units ÷ 500 ml = 40 unit/ml.
(2000 units (dose) ÷ 40 units) x 1 ml = 50 ml/hour
Step 3: Check what the drop factor is on the standard tubing. In this case, the standard tubing is 15 gtt (drops)/ml.
Step 4: Convert the hour to minutes: 1 hour x 60 minutes/hour = 60
Step 5: Input order with converted units into the drip rate formula.
(50 ml ÷ 60 minutes) x (15 gtt ÷ 1 ml)
= (50 ÷ 60 minutes) x (15 gtt)
= 0.833 x 15
= 12.5 drops/minute
= (rounded) 13 drops/minute
BONUS: perhaps you noticed at the beginning that 50ml/hour is more appropriate for micro tubing. The nurse could consider changing to a more appropriate tubing for higher accuracy, particularly if not using an electronic pump.
Drop Factor Mnemonic
One easy way to remember how to calculate drip rate is by using the mnemonic:
“TV will make you deaf over time,” which, if interpreted is:
TV = total volume
Deaf = DF or drop factor
Over = divided by
Time = time prescribed by the physician
We can use this mnemonic using our first example. It’s important to note that the nurse still needs to make the necessary conversions before inputting the numbers into the formula.
Putting the numbers from Example 1 into the formula:
Total Volume (TV) (1,000 ml) x Drop Factor (DeaF) (10 gtt/ml) ÷ Over Time (360 minutes)
= 27.78 drops/min
= 28 gtt/min
This matches the math from Example 1.
As a final word, if you’re ever uncertain about your drip rate, it’s always best to recheck your math if you’re uncertain. Nurses should also use the resources available to them such as pharmacists or their colleagues if they are uncertain about IV calculations.
References
- Wilson K. The nurse’s quick guide to I.V. drug calculations. Nursing Made Incredibly Easy’. Published April 2013. https://journals.lww.com/nursingmadeincrediblyeasy/fulltext/2013/03000/the_nurse_s_quick_guide_to_i_v__drug_calculations.1.aspx
- Harvey M, eBook Nursing Collection – Worldwide. Dosage Calculations Made Incredibly Easy! Fifth;5; Wolters Kluwer Health; 2016. https://go.exlibris.link/pDG3GQ9w