The term “diagnosis” is defined as an agreed-upon clinical judgment. When we think of a diagnosis, it is often thought of as a medical diagnosis, such as hypertension. In its simplest form, a nursing diagnosis is determined by nurses based on their scope and clinical judgment to guide patient care. Nursing diagnoses encompass individuals, families, and communities and relate to health conditions and life processes. Research demonstrates that nursing diagnoses, when appropriately employed, possess greater predictability than medical diagnoses alone in critical aspects such as length of stay and hospital readmission.1
In this article:
- The Nursing Process
- Purpose of a Nursing Diagnosis
- Nursing Diagnoses vs. Medical Diagnoses
- What is NANDA-I?
- Components of a Nursing Diagnosis
- Types of Nursing Diagnoses
- How to Write a Nursing Diagnosis
- Writing a Risk-Focused Diagnosis
- Writing a Health Promotion-Based Diagnosis
- Writing a Syndrome Diagnosis
The Nursing Process
A nursing diagnosis cannot exist without the nursing process; the foundation of nursing practice. Integral to the nursing process is the application of nursing knowledge, encompassing nursing theory, nursing science, and underlying nursing concepts.1 Keep in mind that the nursing process is not always linear and requires adaptability depending on patient data and health outcomes. The nursing process includes these five steps:
Assessment: The nurse collects subjective and objective data about the patient, which may include their physical, emotional, and psychological health, as well as lifestyle factors, socioeconomic status, and culture. Information obtained during the assessment phase may consist of vital signs, activity level, medication use, laboratory values, medical history, and more.
Diagnosis: After the nurse collects and analyzes this data, they can begin to identify actual or potential health problems. This is where nursing diagnoses come into play. The nurse can create a clinical picture to understand possible causes and associations in the patient’s assessment, which will become a part of the patient’s care plan.
Planning: The nurse can now develop a plan and interventions along with short and long-term goals that are individualized to the patient’s needs. In this phase of the nursing process, the nurse also identifies the highest priorities. Urgent or life-threatening physiological conditions will always take precedence, though identified risks may also require prioritization.
Implementation: The nurse puts the plan into action and carries out interventions set in the care plan. Actions are documented for continuity of care.
Evaluation: In the final step of the nursing process, the nurse evaluates the effectiveness of interventions. Goals may be met or may need to be modified. This may require reevaluating one or more steps in the nursing process to revise the care plan based on changes in the patient’s health.
Nursing diagnoses drive actions and allow for continued assessment, prioritization, organization, and effective health outcomes.
Purpose of a Nursing Diagnosis
Nursing diagnoses are used in all care settings and support high-quality, evidence-based care. These are a few ways nursing diagnoses support nursing practice:
- Nursing diagnoses improve collaboration between team members. Nursing diagnoses improve consistency and clarity of communication between nurses and other members of the care team.
- Nursing diagnoses offer a framework for consistent care. Nursing diagnoses include standardized terminology that outlines assessment and interventions, supporting consistent evidence-based practice and clinical decision-making.
- Nursing diagnoses are a teaching tool. For new graduate nurses, familiarity with nursing diagnoses helps to improve critical thinking and confidence in practice. Understanding how nursing diagnoses contribute to the nursing process allows new nurses to become familiar with possible interventions and care pathways for their patients.
- Nursing diagnoses may improve risk identification. Many nursing diagnoses include diagnoses that alert the care team to avoid a potential risk through intervention. For instance, the nursing diagnosis “risk for bleeding” alerts a nurse that the patient may be receiving an anticoagulant and to monitor for signs of bleeding.
- Nursing diagnoses can help establish care goals. Nursing diagnoses illuminate care priorities, including current issues, future risks, and health promotion opportunities. Once the nursing diagnosis is identified, priorities, interventions, and goals can be created in collaboration with the patient.
- Nursing diagnoses promote patient education. Many nursing diagnoses incorporate teaching and opportunities for learning. The nurse may identify knowledge deficits, including medication adherence, health management, nutrition, coping, etc. The nurse utilizes these nursing diagnoses to help patients reach their health and wellness goals.
- Nursing diagnoses serve as documentation. Documentation is crucial in healthcare. If nursing care is not documented, there is no proof it was completed. Documentation of interventions and outcomes provides continuity of care between staff and protects the nurse.
Nursing diagnoses are the foundation of nursing care plans. Nursing diagnoses drive actions and allow for continued assessment, prioritization, organization, and effective health outcomes.
Nursing Diagnoses vs. Medical Diagnoses
Although there are some similarities between medical and nursing diagnoses, such as clinical judgment and shared terminology, they are distinct.2 Physicians utilize the International Classification of Diseases (ICD) taxonomy to denote medical conditions. Mental health professionals such as psychologists or psychiatrists diagnose patients using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). Nurses maintain knowledge of both of these classification systems but instead rely on nursing diagnoses developed by NANDA International, Inc. (NANDA-I).1
Another apparent difference between nursing and medical diagnoses is the healthcare practitioner deciding the diagnosis. All nursing designations share nursing diagnoses, while physicians assign medical diagnoses. The exception is that nurse practitioners in most states can also determine medical diagnoses and prescribe medication. Therefore, a nurse practitioner could determine both nursing and medical diagnoses.
There are also differences in each type of diagnosis. For example, medical diagnoses focus on the disease or pathology that affects the patient. In contrast, nursing diagnoses concentrate on the patient’s response to the illness or life circumstance, which can be either physiological or psychological. By focusing on the client’s response, a nurse applies interventions to address or alter that response.
To clarify this distinction, here are two examples of how medical and nursing diagnoses can work together.
Example 1:
A patient with a medical diagnosis of cerebrovascular accident (stroke) may lead to the complementary nursing diagnosis of Risk for Aspiration. Without the medical diagnosis, the nurse may not know the underlying cause, which could prevent effective planning. The nursing diagnosis is a jumping-off point for creating goals to manage deficits and improve patient safety and quality of life.
Example 2:
With the medical diagnosis of dehydration, the nurse knows that the patient is experiencing Inadequate Fluid Volume (nursing diagnosis). Therefore, the nurse may implement interventions such as administering IV fluids and recording intake and output for this patient.
Nursing and medical diagnoses are complementary and guide each other to create a holistic clinical picture.
What is NANDA-I?
The name NANDA originated as the acronym for the North American Nursing Diagnosis Association. However, with the organization’s global expansion, they no longer use NANDA as an acronym but as a recognizable organizational name. If using the organization’s full name, the correct use is NANDA International, Inc. (no hyphen), and the abbreviation is NANDA-I (with a hyphen). The organization offers networking and education and holds task forces on topics such as diagnosis development, informatics, and nursing research.
Purpose and Mission of NANDA-I
NANDA International is an organization that supports the use and development of standardized nursing terminology throughout clinical settings.3 The organization’s mission is to use nursing diagnoses to promote high-quality patient care through evidence-based research and consistent terminology. Standardized nursing diagnoses inform evidence-based terminology that improves clinical practice by providing clear guidelines for communication and documentation. NANDA International continually releases new editions with revised, added, or retired nursing diagnoses and updates to criteria and classifications.
Components of a Nursing Diagnosis
The following diagnostic indicators guide nurses in applying accurate diagnoses and effective interventions for each patient. A nursing diagnosis does not necessarily require the use of all diagnostic indications.
Diagnosis
Formulating a nursing diagnosis is the second step of the nursing process after assessment.6 First, the nurse analyzes the assessment data collected from patient reports and through observation or diagnostic testing. The nurse will use that data and create clusters of pertinent information to form hypotheses about the appropriate nursing diagnoses. At this stage, the nurse will either write the nursing diagnosis or decide they need additional information to confirm or update their hypothesized diagnosis.
Related Factors
Related factors are the etiology or cause of the nursing diagnosis.4 Related factors are used in problem-focused, syndrome, and sometimes health promotion nursing diagnoses. Related factors are the underlying or contributing conditions or circumstances associated with the patient’s health problem. While the cause may not always be known, the nurse aims to understand the root cause to develop appropriate interventions.
Defining Characteristics
Characteristics and risk factors are the evidence behind the nursing diagnosis.4 However, they should not be used interchangeably. Defining characteristics are observable characteristics that support a problem-focused health promotion diagnosis or syndrome. Defining characteristics are the signs or symptoms of clinical pathology.
Risk Factors
Risk factors are used primarily for risk-focused nursing diagnoses. Risk factors replace the defining characteristics of problem-focused nursing diagnoses. Similarly, they provide supporting evidence for the nursing diagnosis. Unlike defining characteristics, risk factors describe why the patient has an increased chance of acquiring the undesirable health outcome identified by the nurse. Risk factors can be biological, psychological, family, or community-related. Patients may have one or multiple risk factors supporting a risk diagnosis.
At-Risk Populations
The nurse may identify populations that share characteristics that make them susceptible to certain health outcomes. These are non-modifiable by the nurse and may include factors such as age, gender, life events, family history, and more.
Associated Conditions
Medical conditions, surgical procedures, devices, and pharmaceutical agents may relate to a nursing diagnosis. Examples include autoimmune diseases, chemotherapy, oxygen therapy, pregnancy, etc.
Types of Nursing Diagnoses
Problem-Focused
A problem-focused nursing diagnosis is a nursing diagnosis that addresses a current health challenge.4 In contrast to other nursing diagnoses that address potential problems or opportunities for health improvement, a problem-focused diagnosis deals with a current, known health condition. To make this type of diagnosis, the defining characteristics of the diagnosis must be present at the time of evaluation. The defining characteristics include signs, symptoms, and patient health history. Defining characteristics act as clues for the nurse and, when grouped together, form patterns that allow a diagnosis to be assigned. Related factors should also be described as part of a problem-focused nursing diagnosis.
Problem-focused nursing diagnosis example: The nurse notices that the patient has a negative balance between their fluid intake and output. The patient also has dry mucous membranes and weight loss. The nurse makes the problem-based nursing diagnosis of “Inadequate Fluid Volume.” The NANDA-I definition is “Decreased intracellular and/or extracellular fluid, not including blood.” This refers to dehydration, water loss alone without change in sodium.”5 Depending on the etiology and the patient’s health condition, the care plan and interventions will aim to increase fluid intake, identify the cause of the fluid deficit, and maintain evidence of normovolemia.
Health Promotion (Potential to Improve)
In contrast to problem-focused nursing diagnoses, health promotion diagnoses require that the individual/family/community is already functioning effectively in the health area, but there is an opportunity to increase well-being. Another requirement of a health promotion nursing diagnosis is that there is an expressed desire for improvement. This is often expressed at the beginning of the nursing diagnosis statement as “Readiness for enhanced…”. Therefore, the defining characteristic of a health promotion diagnosis is the client/family or community expressing a desire to improve or change health behaviors. There are some similarities to risk-focused nursing diagnoses; however, health promotion diagnoses are further upstream than risk-focused nursing diagnoses, as they aim to improve and actualize health potential instead of preventing an undesirable outcome.
Health promotion nursing diagnosis example: A patient expresses the desire to breastfeed exclusively during a prenatal screening visit with a nurse. The nurse recognizes the opportunity for health promotion with the nursing diagnosis of “Readiness for Enhanced Chestfeeding.” The NANDA-I definition is a “Pattern of providing human milk to an infant or child, which can be strengthened.”5 Based on this assessment, the nurse may refer the client to trusted online sources of information or refer them to a lactation consultant.
Risk-Focused (Potential to Deteriorate)
In a risk-based diagnosis, the nurse uses their clinical judgment to determine that the patient is at risk for health consequences if preventative measures are not implemented. Otherwise stated, the problem has not yet manifested for the client/family/community, but there is a vulnerability related to risk factors that the nurse identifies. Care plans will focus on preventing undesirable health outcomes.
Risk-focused nursing diagnosis example: In an inpatient surgical unit, a nurse is assigned to a patient postoperative day 3 for Whipple surgery. This nurse immediately recognizes that the patient meets the criteria for the nursing diagnosis of “Risk for Infection.” The NANDA-I definition is “Susceptible to invasion and multiplication of pathogenic organisms.” This patient is at risk due to their diagnosis of pancreatic cancer and recent surgery. One intervention the nurse may invoke is patient teaching on handwashing and providing the patient with alcohol-based antiseptic hand rub on their bedside table.
Syndrome
Nursing diagnosis syndromes are created when two or more concurrent nursing diagnoses are related and can be treated using similar interventions. Nursing syndrome diagnoses also cluster problem and risk-focused nursing diagnoses that often accompany specific health processes or life events.
Syndrome nursing diagnosis example: A patient shares that they recently witnessed a motor vehicle accident resulting in multiple injuries, including deaths. While not injured, they report difficulties sleeping, increased alcohol use, and irritability, which are now beginning to impact their ability to work. The nurse recognizes this cluster of symptoms as consistent with the nursing diagnosis of “Post-Trauma syndrome.” The NANDA-I definition of Post-Trauma Syndrome is a “Sustained maladaptive response to a traumatic, overwhelming event.” 5 Other nursing diagnoses that may cluster to form this syndrome include “Ineffective Sleep Pattern,” “Excessive Anxiety,” “and “Maladaptive Coping.” The nurse discusses the goal of acknowledging the trauma and discusses options to connect the patient to support resources.
How to Write a Nursing Diagnosis
Standardized methods of writing nursing diagnoses allow for clear communication of their purpose and driving factors. Writing a complete nursing diagnosis helps the nurse clarify their reasoning for potential interventions and care goals.
Writing a Problem-Focused Nursing Diagnosis
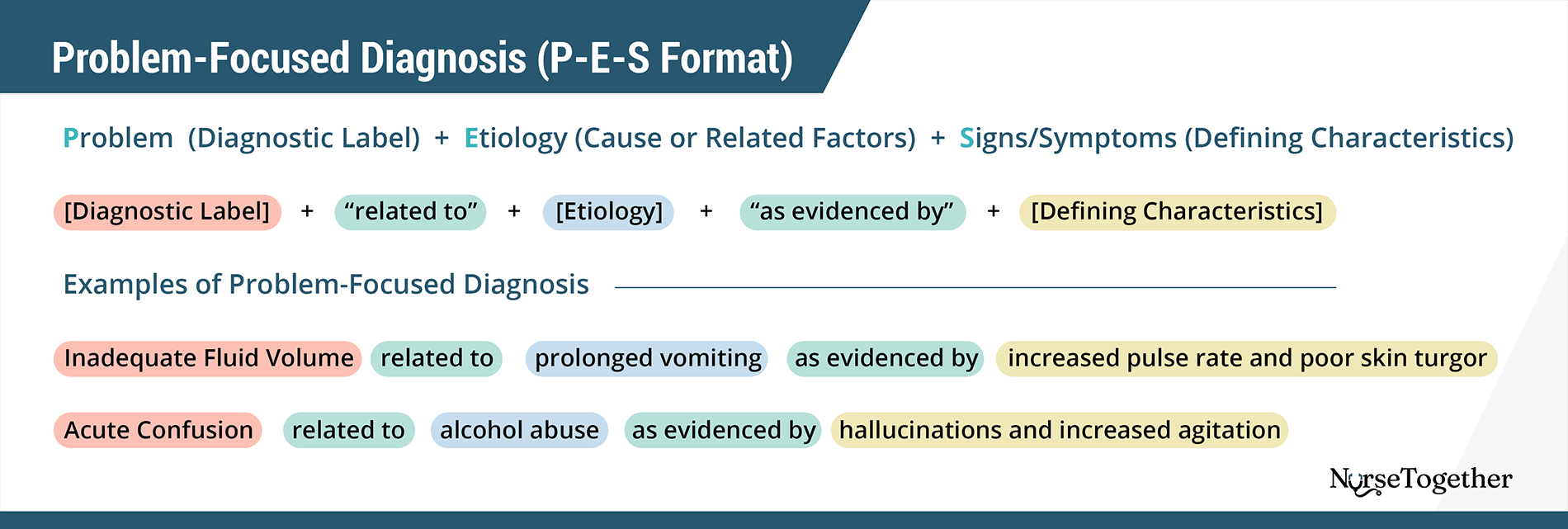
Problem-focused nursing diagnoses are three-part statements that include the problem, etiology, and symptoms (PES framework).
How to write a Problem-Focused Diagnosis (P-E-S Format)
Problem (Diagnostic Label) + Etiology (Cause or Related Factors) + Signs/Symptoms (Defining Characteristics)
[Diagnostic Label] + “related to” + [Etiology] + “as evidenced by” + [Defining Characteristics]
Examples of Problem-Focused Diagnosis:
Inadequate Fluid Volume related to prolonged vomiting as evidenced by increased pulse rate and poor skin turgor.
Acute Confusion related to alcohol abuse as evidenced by hallucinations and increased agitation.
Problem (Nursing Diagnosis)
Nurses should use a NANDA-I label whenever possible to describe the identified problem to ensure consistency in diagnoses. However, if no NANDA-I label adequately represents the problem, the nurse needs to describe the problem in a clear, concise, and useful way to the care team. It is important to avoid judgmental language in the problem statement.
Etiology (Related Factors)
The second part of the problem-focused nursing diagnosis is the etiology or the underlying cause or causes of the nursing diagnosis. The etiology of the diagnosis is key to choosing appropriate interventions, so the nurse should describe the etiology as precisely as possible. For instance, what was the event’s timing, or how long has the client had the disease? When describing an etiology linked to a known pathophysiology or disease, the etiology should be stated as “secondary to.” Otherwise, the etiology should be stated as “related to” (R/T). “Related to” does not necessarily specify a direct cause-and-effect relationship, which is preferred because there may be other factors related to the nursing diagnosis that have not yet been identified.
When various factors contribute to a nursing diagnosis that cannot be summarized into a one-sentence statement, the etiology may be written as “related to complex factors.” This should not be used as a shortcut to finding the appropriate etiology, but when there is no clear primary etiology for the nursing diagnosis.
Signs/Symptoms (Defining Characteristics)
For a problem-focused nursing diagnosis, the described signs and symptoms are the defining characteristics of the nursing diagnosis. The nurse should link the etiology to the signs and symptoms by stating “as manifested by” (AMB) or “as evidenced by” (AEB).
Writing a Risk-Focused Diagnosis
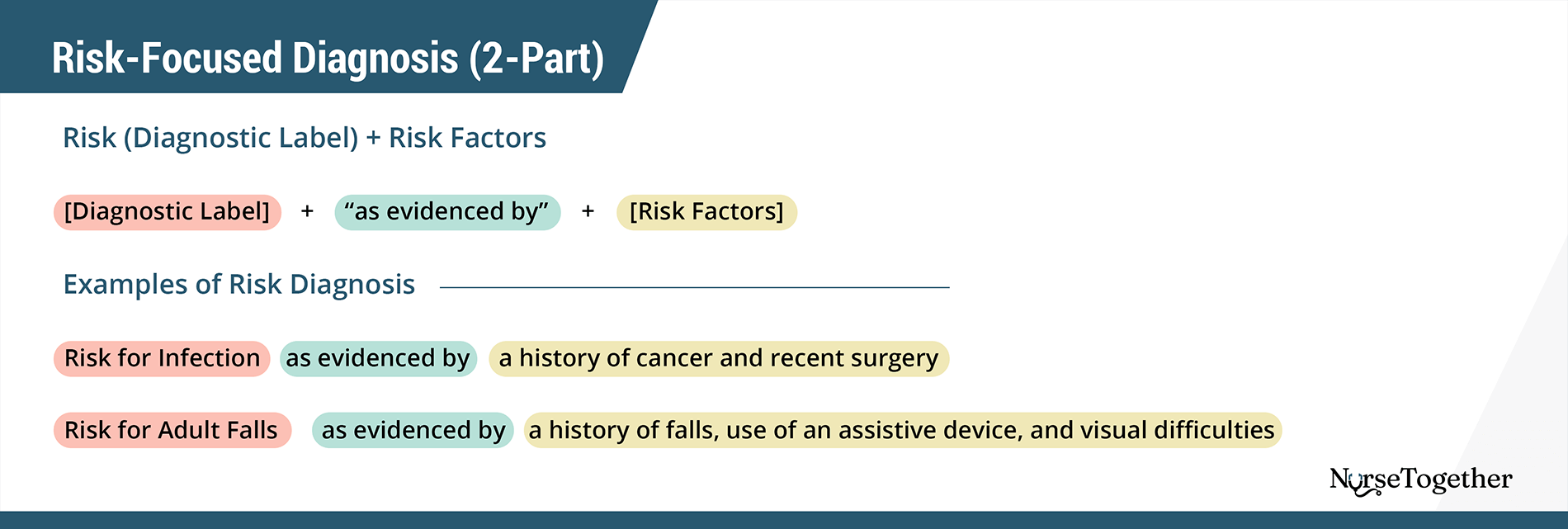
The risk-focused diagnosis is a two-part statement that includes statements of the problem and risk factors.
How to write a Risk-Focused Diagnosis
Risk (Diagnostic Label) + Risk Factors
[Diagnostic Label] + “as evidenced by” + [Risk Factors]
Examples of Risk Diagnosis:
Risk for Infection as evidenced by a history of cancer and recent surgery.
Risk for Adult Falls as evidenced by a history of falls, use of an assistive device, and visual difficulties.
Problem (Nursing Diagnosis)
Like a problem-focused diagnosis, the risk-focused statement should also use a NANDA-I approved diagnosis starting with “Risk for…”. If a NANDA-I nursing diagnosis does not adequately describe the vulnerability, the nurse should still begin their problem statement with “Risk for…”.
Risk Factors
Rather than describing the etiology or related factors, risk-focused diagnoses are supported by describing the risk factors related to the diagnosis. The risk factor statement should follow the problem statement with the nurse describing the problem “as evidenced by” and then listing the risk factors.
Defining characteristics are not possible because they haven’t actually occurred yet.
Writing a Health Promotion-Based Diagnosis
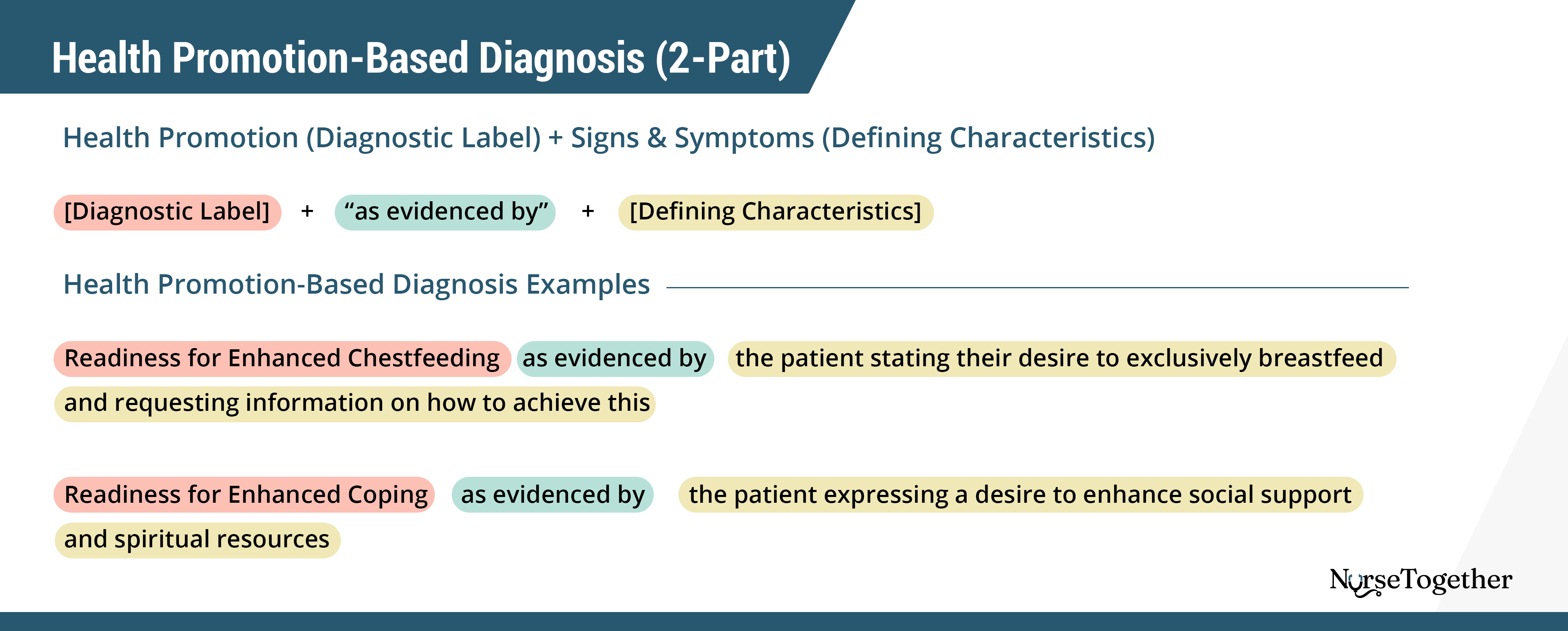
A health promotion diagnosis is also described using a two-part statement.
How to write a Health Promotion-Based Diagnosis (2-Part)
Health Promotion (Diagnostic Label) + Signs & Symptoms (Defining Characteristics)
[Diagnostic Label] + “as evidenced by” + [Defining Characteristics]
Health Promotion-Based Diagnosis Examples:
Readiness for Enhanced Chestfeeding as evidenced by the patient stating their desire to exclusively breastfeed and requesting information on how to achieve this.
Readiness for Enhanced Coping as evidenced by the patient expressing a desire to enhance social support and spiritual resources.
Problem (Nursing Diagnosis)
Rather than identifying a health problem, the nurse recognizes an opportunity to improve the patient’s health outcomes. When possible, the nurse should use an approved NANDA-I health promotion diagnosis. If the nurse is formulating their own problem statement for a health promotion diagnosis, they should start the statement with “Readiness for enhanced…”.
Signs/Symptoms (Defining Characteristics)
The signs and symptoms used to describe a health promotion diagnosis are related to the patient, family, or community expressing readiness or desire for health improvement. This may be a verbal expression, actions, or other cues that alert the nurse to readiness for health promotion.
Writing a Syndrome Diagnosis
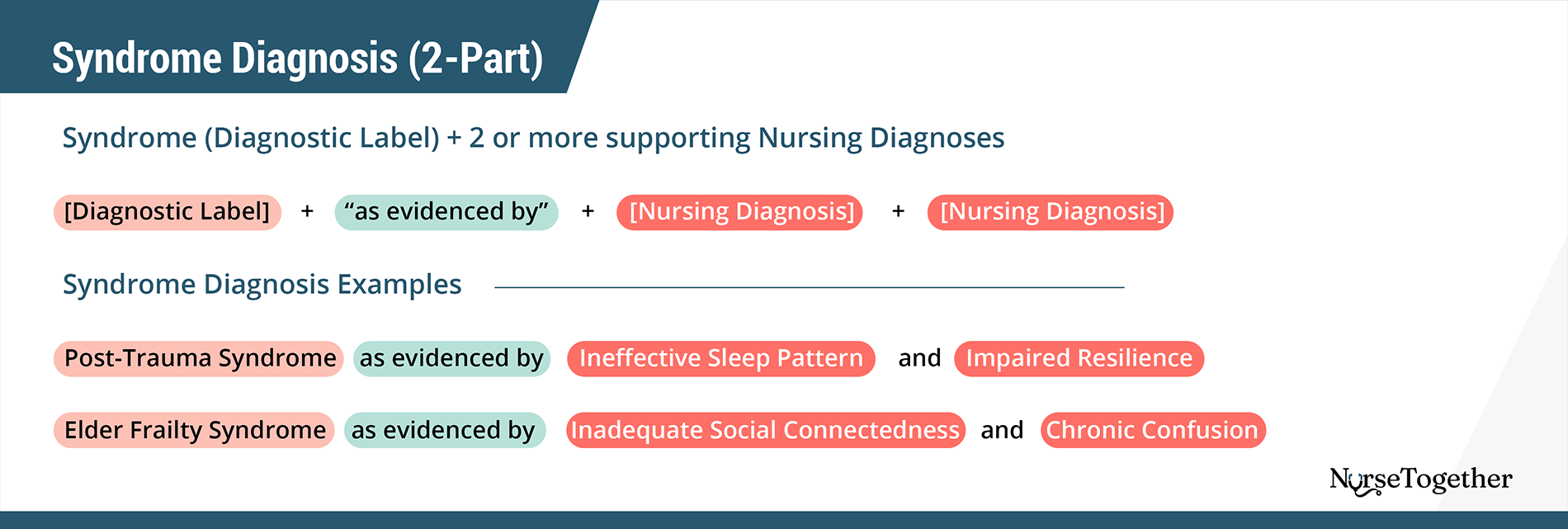
The syndrome diagnosis is a group of related nursing diagnoses and should be written as a two-part statement.7
How to write a Syndrome Diagnosis (2-Part)
Syndrome (Diagnostic Label) + 2 or more supporting Nursing Diagnoses
[Diagnostic Label] + “as evidenced by” + [Nursing Diagnosis] + [Nursing Diagnosis]
Syndrome Diagnosis Examples:
Post-Trauma Syndrome as evidenced by Ineffective Sleep Pattern and Impaired Resilience.
Elder Frailty Syndrome as evidenced by Inadequate Social Connectedness and Chronic Confusion.
Problem (Nursing Diagnosis)
The nurse should use a recognized NANDA-I syndrome to diagnose a nursing syndrome.
Etiology (Additional Nursing Diagnoses)
For a syndrome diagnosis, the etiology is described as two or more nursing diagnoses that form the evidence for the syndrome diagnosis. There should be a minimum of two diagnoses, with no maximum of nursing diagnoses to support a syndrome diagnosis. Each nursing diagnosis should be written in its complete, appropriate form, either including etiology, signs and symptoms, or risk factors.
List of Current Nursing Diagnoses and Domains
In the 2024 to 2026 edition of NANDA-International Nursing Diagnoses, there are 13 domains of nursing diagnoses. Each domain is divided into classes of nursing diagnoses that are then broken down into individual diagnoses. Here, we list all 13 domains, related classes, and an example of a nursing diagnosis. Please refer to NANDA-International Nursing Diagnoses Definitions and Classification, 13th Edition, for the complete list of updated diagnoses.
Domain 1: Health Promotion
Class 1: Health Awareness
Class 2: Health Management
Diagnosis: Readiness for Enhanced Health Self-Management
Domain 2: Nutrition
Class 1: Ingestion
Class 2: Digestion
Class 3: Absorption
Class 4: Metabolism
Class 5: Hydration
Diagnosis: Inadequate Nutritional Intake
Domain 3: Elimination and exchange
Class 1: Urinary function
Class 2: Gastrointestinal function
Class 3: Integumentary function
Class 4: Respiratory function
Diagnosis: Risk for Urinary Retention
Domain 4: Activity/rest
Class 1: Sleep/Rest
Class 2: Activity/Exercise
Class 3: Energy balance
Class 4: Cardiovascular/Pulmonary responses
Class 5: Self-care
Diagnosis: Decreased Activity Tolerance
Domain 5: Perception/cognition
Class 1: Attention
Class 2: Orientation
Class 3: Sensation/Perception
Class 4: Cognition
Class 5: Communication
Diagnosis: Impaired Memory
Domain 6: Self-perception
Class 1: Self-concept
Class 2: Self-esteem
Class 3: Body image
Diagnosis: Chronic Inadequate Self-Esteem
Domain 7: Role relationship
Class 1: Caregiving roles
Class 2: Family relationships
Class 3: Role performance
Diagnosis: Impaired Social Interaction
Domain 8: Sexuality
Class 1: Sexual identity
Class 2: Sexual function
Class 3: Reproduction
Diagnosis: Risk For Disturbed Maternal-Fetal Dyad
Domain 9: Coping/stress tolerance
Class 1: Post-trauma responses
Class 2: Coping responses
Class 3: Neurobehavioral stress
Diagnosis: Excessive Caregiving Burden
Domain 10: Life principles
Class 1: Values
Class 2: Beliefs
Class 3: Value/Belief/Action congruence
Diagnosis: Moral Distress
Domain 11: Safety/protection
Class 1: Infection
Class 2: Physical injury
Class 3: Violence
Class 4: Environmental hazards
Class 5: Defensive processes
Class 6: Thermoregulation
Diagnosis: Risk for Surgical Wound Infection
Domain 12: Comfort
Class 1: Physical comfort
Class 2: Environmental comfort
Class 3: Social comfort
Diagnosis: Acute Pain
Domain 13: Growth/development
Class 1: Growth
Class 2: Development
Diagnosis: Delayed Infant Motor Development
List of Common Nursing Diagnoses
In this section, you will find common NANDA-I nursing diagnoses along with care plan examples.
Note: Nursing diagnoses are revised, added, or retired by the NANDA International Diagnosis Development Committee (DDC) to coincide with shifts in language standardization. Students and seasoned nurses alike may be unfamiliar with recent changes, and thus NurseTogether has chosen to continue to utilize potentially outdated or retired nursing diagnoses but will apply updated or new wording as applicable, such as in the diagnoses found below in parentheses.
- Activity Intolerance (Decreased Activity Tolerance)
- Acute Confusion
- Acute Pain
- Anxiety (Excessive Anxiety)
- Chronic Pain
- Constipation (Chronic Functional Constipation)
- Decreased Cardiac Output (Risk For Decreased Cardiac Output)
- Diarrhea (Impaired Fecal Continence)
- Disturbed Body Image (Disrupted Body Image)
- Excess Fluid Volume (Excessive Fluid Volume)
- Fatigue (Excessive Fatigue Burden)
- Fluid Volume Deficit (Inadequate Fluid Volume)
- Hopelessness (Impaired Resilience)
- Hyperthermia
- Imbalanced Nutrition (Inadequate Nutritional Intake)
- Impaired Comfort (Impaired Physical Comfort/Impaired Psychological Comfort)
- Impaired Gas Exchange
- Impaired Physical Mobility
- Impaired Skin Integrity
- Impaired Urinary Elimination
- Impaired Verbal Communication
- Ineffective Airway Clearance
- Ineffective Breathing Pattern
- Ineffective Coping (Maladaptive Coping)
- Ineffective Health Maintenance (Ineffective Health Self-Management)
- Ineffective Tissue Perfusion (Ineffective Peripheral Tissue Perfusion)
- Insomnia (Ineffective Sleep Pattern)
- Knowledge Deficit (Inadequate Health Knowledge)
- Noncompliance/Ineffective Adherence (Retired)
- Risk For Aspiration
- Risk for Bleeding (Risk For Excessive Bleeding)
- Risk for Electrolyte Imbalance (Risk For Impaired Water-Electrolyte Balance)
- Risk for Falls (Risk For Adult/Child Falls)
- Risk for Infection
- Risk for Injury (Risk For Physical Injury)
- Risk For Unstable Blood Glucose (Risk For Ineffective Blood Glucose Pattern Self-Management)
- Self-Care Deficit (Decreased Self-Care Ability Syndrome)
- Social Isolation (Inadequate Social Connectedness)
- Stress Overload (Retired)
- Urinary Retention (Risk For Urinary Retention)
References
- Herdman, T. H., Kamitsuru, S., & Lopes, C. (Eds.). (2024). NANDA-I International Nursing Diagnoses: Definitions and Classification, 2024-2026. Thieme. 10.1055/b000000928
- NANDA Internatioal. What is the difference between a medical diagnosis and a nursing diagnosis? Accessed January 7, 2023. http://nanda.host4kb.com/article/AA-00266/0/What-is-the-difference-between-a-medical-diagnosis-and-a-nursing-diagnosis-.html
- NANDA Internatioal. Our Story. Accessed January 7, 2023. https://nanda.org/who-we-are/our-story/
- NANDA Internatioal. Glossary of Terms. Accessed January 3, 2023. https://nanda.org/publications-resources/resources/glossary-of-terms/
- Carpenito LJ, Books@Ovid Purchased eBooks. Handbook of Nursing Diagnosis. 15th ed. Wolters Kluwer; 2017.
- Open Resources for Nursing. DIAGNOSIS. In: Nursing Fundamentals.
- NANDA Internatioal. The Structure and Development of Syndrome Diagnoses. Accessed January 7, 2023. https://nanda.org/publications-resources/resources/position-statement/